
The failure to make progress against Alzheimer’s disease over the last 20 years has forced governments, academia and the pharma industry to think outside the box.
A dispiriting string of late stage failures in pharma suggest the same mistakes are being made over and over again: not enough fundamental understanding of the disease, inadequate sharing of pre-competitive data, trial recruitment problems, and trial design that is ill-suited to making rapid progress against this elusive disease.
The last few years have seen the launch of numerous public-private partnerships in translational research partnerships which aim to bridge these gaps and raise the chances of success by pooling resources.
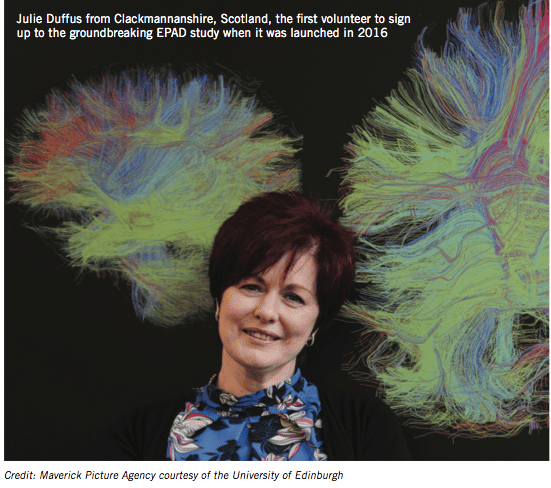
One of the most notable is the European Prevention of Alzheimer’s Dementia (EPAD) project, an interdisciplinary research consortium that aims to improve understanding of the early stages of Alzheimer’s disease and deliver new preventative treatments.
EPAD is co-funded by the Innovative Medicines Initiative (IMI) and Europe’s pharma industry organisation EFPIA, and 2019 will see the first patients being treated by this groundbreaking new alliance.
The EPAD platform will allow new therapies to be tested in a streamlined way, using adaptive trial design to test more targeted interventions and select only those patients most likely to benefit from treatments to slow or stop dementia.
EPAD combines knowledge and expertise from 39 European partner organisations across multiple sectors, including most of the big pharma companies involved in Alzheimer’s research (including Amgen, Janssen and Lilly, among others) and universities across six European countries, from Edinburgh in Scotland to Zaragoza in Spain.
EPAD has three pillars:
1. The Register: EPAD has created the first single, pan-European register of over half a million people across the risk spectrum for dementia.
2. The Cohort: From this register, research participants are invited to join an EPAD cohort of at-risk subjects, the Longitudinal Cohort Study, known as the LCS. This group will undergo standardised tests and follow-up over several years.
3. The Trial: EPAD will select participants to take part in streamlined proof-of-concept (PoC) trials of drugs designed to prevent Alzheimer’s dementia. These trials aim to accommodate phase 2-ready small molecule or biologic candidates.
The consortium is now preparing to launch the new trial delivery centres (TDCs) to put the EPAD Longitudinal Cohort Study (LCS) into action.
Prof Craig Ritchie is Professor of the Psychiatry of Ageing at the University of Edinburgh and leader of the EPAD consortium.

Prof Craig Ritchie
“EPAD is part of a global initiative that will make a fundamental difference to the understanding and management of Alzheimer’s disease in people with very early symptoms, or no symptoms at all. This could be a game changer.
It is only possible because of the absolute commitment of academics, industry, policymakers and the public to work hand-in-hand to defeat this global threat.”
This project has numerous advantages over current approaches. These include the excellent pre-trial characterisation of research participants to inform selection and reduce screen failure, the establishment of the highest possible quality study sites across Europe, the rapid decision-making on the likely success of a drug (or combination of drugs) in subsequent confirmatory trials, as well as access to a shared placebo group.
The venture capital approach to dementia research
The Dementia Discovery Fund is a venture capital fund focused on discovering and developing novel therapies for dementia, first set up in October 2015.
The global consortium aims to take a biotech venture capital style approach to Alzheimer’s research, and recently saw its first investment come to fruition.
US biotech company Alector, which is pioneering work in immuno-neurology and novel therapeutic approaches to treating neurodegeneration, raised $176m in an initial public offering in early February.
Alector was the DDF’s first investment in 2015, and is one of 16 companies and translational projects in which the DDF has invested to date.
Alector has devoted the last five years to the development of novel therapeutics that harness the brain’s immune system to treat neurodegeneration, identifying over 40 immune system targets, progressing more than ten programmes into preclinical research and advancing two product candidates, AL001 and AL002, into clinical development.
AL001, initially aimed at treating a genetically defined subpopulation of patients with frontotemporal dementia (FTD), has demonstrated phase I proof-of-mechanism in the central nervous systems of healthy volunteers, with further data expected this year. A phase I dose escalation study of AL002 for patients with Alzheimer’s disease, as part of a global strategic partnership with AbbVie, is ongoing. Two further candidates, AL003 for Alzheimer’s disease and AL004 for multiple degenerative disorders, are also set to enter clinical trials this year.
Angus Grant, CEO of the Dementia Discovery Fund, said: “I am delighted that Alector, the first of DDF’s investments, has reached this significant milestone. It is testament to the company’s innovative science and novel approach to developing future treatments for dementia.
“Alector’s progress serves as a great illustration of how the DDF’s investment choices can contribute to furthering the field of neuroscience research. The development of immunotherapies has, in recent years, dominated our progress in tackling cancer and Alector’s approach in harnessing the power of the immune system to target neurodegeneration was a compelling investment opportunity for the DDF.”
Jean Georges Executive Director of Alzheimer Europe: “Preventing the development of dementia in biomarker-positive people would be a fantastic step forward in our fight against Alzheimer’s disease. The EPAD and its novel trial concept will hopefully help speed-up the drug discovery progress and bring us closer to this ambitious aim.”
Luc Truyen, Vice President, Neuroscience External Affairs at Janssen R&D said that failures in the field pointed towards a need to target Alzheimer’s disease earlier in its progression.
“We see there is an opportunity to affect the disease early before significant damage is done and give these disease-modifying drugs a chance to show what they can do.
“Number one is identifying accurately that population in terms of who would benefit most from pharmacological intervention. And the second main challenge is then how one makes decisions on outcomes, as to whether drugs are effective in a population that may well be entirely asymptomatic.”
Funding for EPAD from IMI comes to an end in late 2019, but now that the infrastructure is in place, the partners hope to continue the initiative for many years to come.
By early March 2019, there were 21 study sites up and running, with 1,494 research participants recruited.
Katrin Haeverans, EPAD LCS and POC platform support, Janssen said: “EPAD has been built to facilitate proof-of-concept trials. We started a few years ago and these are really exciting times, because now we have many sites up and running to do phenotyping of their
subjects, who ultimately might go into a POC trial. These are really exciting times because now we have built the platform to facilitate a quick start-up for these POC trials.”
The first proof-of-concept trial is expected to start in 2019 or 2020, and will include three interventions in different arms.
Pioneering adaptive trials for Alzheimer’s
The case for using adaptive trials against dementia is clear: by generating better data and improved decision-making, adaptive trials can increase the probability of success and decrease development time.
Adaptive clinical trials dispense with the classical placebo-controlled design, and instead tests candidate drugs simultaneously compared to each other and to a placebo.
This allows a greater proportion of patients to potentially benefit from new therapies. It also allows researchers to adapt the trial design in response to emerging results, add new candidate drugs and abandon those that prove to be ineffective.
By setting up a trial-ready cohort of research participants, creating a pan-European network of trial sites, identifying ineffective medicines earlier in the development process and eliminating failures in more advanced (phase 3) trials, EPAD aims to accelerate the development of effective therapies.
|
The Dementia Consortium |
|
The Dementia Consortium is another initiative aimed at breaking down the barriers within the research world that prevent faster progress being made. Led by the British dementia research charity, Alzheimer’s Research UK, it aims to bring together academic researchers with pharma and biotech to accelerate the development of novel treatments. Last month, Johnson & Johnson Innovation, Takeda and Evotec became the latest pharma research groups to join the initiative, alongside existing strategic partners AbbVie, Astex Pharmaceuticals, Eisai, Lilly and MSD. The Dementia Consortium provides academic researchers with the funding, industry expertise and project management resources to capitalise on new drug targets for the treatment of the neurodegenerative diseases that cause dementia. Diseases include Alzheimer’s, dementia with Lewy bodies, frontotemporal dementia, as well as Parkinson’s and Huntington’s disease. Dr Carol Routledge, Director of Research at Alzheimer’s Research UK, said: “We’re excited to welcome Johnson & Johnson Innovation, Takeda Pharmaceuticals and Evotec to the Dementia Consortium as we look to build on the excellent work it has achieved so far. The Dementia Consortium will give new opportunities for world-leading academic researchers to develop their novel and promising findings into treatments. Supporting these projects is vital in helping make scientific breakthroughs possible and bringing about a new life-changing dementia treatment.” The collaboration provides a cost and risk sharing approach to robust target validation and catalyses the collaboration between academic researchers, charity and pharmaceutical companies to translate novel drug targets towards the clinic. The Dementia Consortium is already supporting seven pioneering projects, with more expected to follow. Examples of ongoing projects include two which target the immune system with an aim to halt nerve cell damage in Alzheimer’s and Parkinson’s and another which investigates the role of a protein called TDP-43 that builds up in the brains of people with frontotemporal dementia and motor neurone disease. The Dementia Consortium is currently accepting applications for innovative new dementia targets with a rolling deadline for expressions of interest every three months. Successful projects may then be considered for licensing to industrial partners to facilitate the progression of novel treatments into the clinic.
Sir Simon Lovestone After 18 years in old age psychiatry and dementia research in academia, Sir Simon Lovestone joined Janssen at the end of 2018. He is now Neurodegeneration Disease Area Stronghold Leader at Janssen Research & Development, and his background in academic research makes him an ideal partner to bridge the gap between early research and commercial drug development. “We are delighted to collaborate as part of the Dementia Consortium, and we believe this is an exciting approach to identify novel targets for drug discovery in neurodegeneration, with the ultimate goal of helping patients all over the world who suffer from debilitating central nervous system disorders.” |





