Resistance to antibiotic medicines will account for 10 million extra deaths a year by 2050 if action isn’t taken, according to a UK report.
The first paper from the five-year Review on Antimicrobial Resistance, led by Jim O’Neill, estimates a huge rise on the current figure of 700,000 deaths per year as infections grow immunity to treatments. Developing nations in Asia and Africa will be hardest hit.
The cost of tackling antimicrobial resistance will also rise, according to the review, hitting $100trn in 36 years time, with the rise of E. coli, malaria and tuberculosis set to have the biggest impact.
The UK strategy was launched in 2013 based on recommendations made by chief medical officer Dame Sally Davies, highlighting the need to improve the commercial viability of new antibiotics and encourage responsible use of existing drugs.
It was followed in July this year by the launch of a review into how to improve the research and regulatory environment for companies working in the development of antibiotics, which has been seen as an area of little interest for many pharma companies due to the poor return on investment of antibiotics.

England’s chief medical officer Dame Sally Davies is leading a call to improve the antibiotic research environment for pharma companies
One year on from the launch of the UK 5 Year Antimicrobial Resistance (AMR) Strategy the first progress report has been published, with indications that – despite there being a long way to go – things are improving.
“A year further on, we have put antimicrobial resistance securely on the international agenda,” said Dame Sally in her foreword to the update. “We hope the alliances we have built, working closely with governments and partners across human and animal health, will help to ensure there is a sustained global commitment to take action.”
Specific progresses highlighted by the report include new prescribing measures that aim to reduce total antibiotic prescribing and encourage the use of narrow spectrum antibiotics in both primary and secondary care.
This is set to be strengthened by guidance in development by the National Institute for Health and Care Excellence (NICE) on the use of antibiotics.
Other positives noted by the report include the identification of new approaches to deliver change in GP and public behaviour following a review into the best ways to influence both public and professional behaviour with regard to the prescribing and use of antibiotics.
The UK and Sweden has also led the development and adoption of a new World Health Organisation (WHO) Resolution on antimicrobial resistance, which provides a mandate for the development of a WHO-led Global Action Plan by May 2015.
“Together, these achievements form a valuable basis from which to progress the work set out in the implementation plan,” says the report.
The progress report was welcomed by Public Health England, which is leading on four elements of the strategy, although its director for international public health Prof Anthony Kessel warned of the difficulties going forward.
“If ever we needed a reminder of what a public health catastrophe looks like then this has to be it,” he said.
“Stopping resistance developing should be straight forward: prescribing the right antibiotic for the right infection for the right time and stopping infections spreading by practicing good infection control. However, in reality this can be difficult to achieve, particularly in countries where antibiotics are freely available or there is lack of sanitation and healthcare is limited.
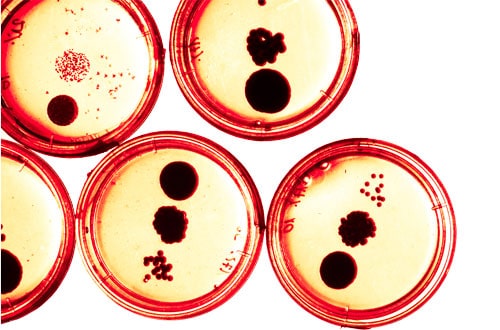
“Given that bacteria can grow and mutate at a considerable rate, we have to be swift and decisive in our response.”




