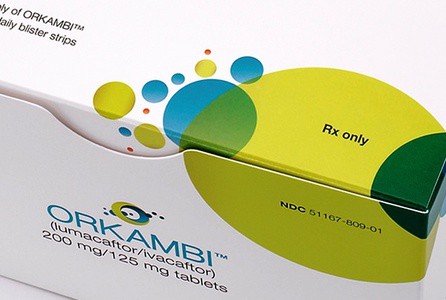
The opposing sides in the long-running dispute over access to cystic fibrosis treatment Orkambi will come face-to-face at a public meeting on Thursday as a parliamentary inquiry gets under way.
Vertex’s CEO Jeff Leiden will fly into London from the US to appear at the House of Commons’ health and social care committee inquiry, and will follow directly after NHS England’s National Director of Specialised Commissioning, John Stewart, in facing tough questions from the panel of MPs about Orkambi access on the NHS.
The two sides have failed to reach a deal since Orkambi was first granted marketing approval across Europe in November 2015.
An increasingly entrenched and public row over the drug’s price has left eligible patients and their families desperate for a breakthrough – and angry at both Vertex and NHS England.
The Commons’ committee has published written submissions from a number of stakeholders, ranging from the UK biotech association the BIA, rare disease campaign group Genetic Alliance, David Turner, a barrister, CF campaigner and father of a teenage daughter with the condition, The CF Trust and new patient action group Just Treatment.
Submissions from NHS England (NHSE) Vertex and NICE haven’t been released in advance of the hearing, however.
The stakeholder submissions show a common urgency to find a solution to the long-running problem – as Orkambi could prevent life-threatening infections taking hold – there is no clear consensus on where the blame lies for the impasse, or exactly how a deal could be reached, but there is some convergence around possible longer-term solutions.
Most stakeholders identify Orkambi as an urgent and exceptional problem, but also part of a wider problem in England over access to medicines for rare and ultra-rare conditions.

Vertex’s CEO Jeff Leiden will have to defend Vertex pricing strategy
From an industry perspective, the BIA’s submission argues that shortcomings in NICE and NHSE’s methodologies for assessing rare and ultra-rare diseases are the root problem. They say other countries have developed more agile systems – citing France ‘Temporary Authorisation for Use (ATU) for novel rare disease treatments.
Patients can access the product immediately while a price is agreed between the manufacturer and the healthcare system. If a budget impact cap of €30m per year is breached, then the average price per patient per year must be lower than €10,000.
It says these and other examples from European systems could provide answers.
The BIA submission concludes: “[We] believe that a systemic challenge exists that requires a systemic solution. If this is not developed, we fear that rare disease patients in England will continue to be left behind, and disputes between NHS England, NICE and producers of innovative medicines will become more common.”
The long-running row, and Vertex’s apparent inflexibility on its price, has hardened sentiment against it and the industry, however. This has led to the creation of Just Treatment, a new patient action group which is advocating the compulsory licensing of Vertex to break the deadlock, so-called Crown use licensing.
It says: “Vertex’s claims that a Crown use licence would significantly undermine future innovation do not stand up to scrutiny. In the face of Vertex’s corporate intransigence, the lives of NHS patients should take precedent.”
However, health minister Steve Brine indicated in Parliament last month that it was very unlikely to use this route, as it would involve paying compensation to Vertex.
In his submission, barrister David Turner provides a forensic dissection of NHS England and Vertex’s negotiations to date – including pointing out a great contrast between the speed of a deal agreed for Vertex’s first CF drug, Kalydeco in 2012 and the more ‘hardnosed’ NHSE approach taken with Orkambi.
Nonetheless, he says: “The principal reason for the current impasse is Vertex’s approach to pricing. Those within the company who might moderate Vertex’s behaviour are disincentivised from doing so. It is doubtful that Vertex’s behaviour would change unless its continuation had a marked and adverse impact upon its share price.”
However, he doesn’t spare NHS England from criticism, saying it is practising “genetic discrimination” and failing on its promise to provide high quality care for all patients.
Vertex has rejected NHS England’s “last and final deal,” which offered the company guaranteed revenues of £500m over the next five years and £1bn over 10 years for all of its cystic fibrosis drugs.
Turner says NHS England were ‘disingenuous’ in demanding that Vertex publish its offer price for Orkambi, and in making public its formerly confidential offer. Turner argues that the price negotiations are confidential by their nature, and making them public makes it impossible for Vertex to accept them.
“The unavoidable inference is that NHS England and the ministers who trumpeted the offer were simply posturing in the hope of eliciting favourable media treatment; they did so without regard to the emotions of cystic fibrosis patients or members of the wider cystic fibrosis community.”
Turner says three changes need to be introduced for the future: immediate patient access to medicines under review; a license holder able to appeal (to a specialist body) against an adverse decision; binding arbitration (as used in Germany) to resolve disputes over cost between NHS England and a licence holder.
It’s not clear what kind of tone the adversaries will strike in their testimony on Thursday; NHSE’s John Stewart has accused Vertex of being ‘extreme outliers’ while Vertex’s Jeff Leiden has called the health service organisation’s stance ‘outrageous’.
Both sides know that inflammatory language won’t look good in personal testimony – but whether the public scrutiny can produce a breakthrough is yet to be seen.
Patient campaigners stress that CF patients ‘haven’t got the luxury of time‘ for negotiations to drag on any longer, so any deal to provide interim access to eligible patients would be seen as a major victory – though this kind of arrangement is currently limited in England to the Cancer Drugs Fund.
Read the written submissions to the health and social care committee here.




