3D printing went beyond its theoretical applications in the pharma industry when the first drug manufactured using the technology was approved by the FDA. But just how broadly will this form of additive manufacturing be used by drugmakers?
PME has previously examined the potential for 3D printing across the healthcare spectrum – spanning the production of bespoke implants and prostheses, early work on developing scaffolds for replacement tissues and organs and as training aids for surgeons, among other uses.
In this article we focus on the technology’s potential for drug manufacturing, formulation and delivery systems, for example creating medicines with release profiles that are unachievable with current approaches and ‘polypills’ that can deliver multiple active drugs, either as a blend or in different compartments of the tablet.
First approved medicine
At the moment, oral tablets are prepared via well-established processes such as mixing, milling, and dry and wet granulation of powdered ingredients that are formed into tablets through compression or moulds.
The approval of Aprecia Pharmaceuticals’ new epilepsy drug Spritam (levetiracetam) in August was a landmark because it marked the first time that 3D printing was deployed as an alternative production method in a commercially-available pharmaceutical product.
The drug is made using Aprecia’s ZipDose platform, a powder jet system that allows the active pharmaceutical ingredients (APIs) and excipients in each tablet to be produced layer by layer.
The platform has a simple objective – making tablets that dissolve much more rapidly than is possible using conventional tableting techniques and are small, even if the dose of the drug required is high. The company says it can incorporate up to 1,000mg of drug in a single dose using the technology, and also bundle in taste-masking compounds for bitter compounds.
“Spritam is designed to fill a need for patients who struggle with their current medication experience,” commented Don Wetherhold, Aprecia’s chief executive. “This is the first in a line of central nervous system products Aprecia plans to introduce as part of our commitment to transform the way patients experience taking medication.”
Getting regulatory approval for the drug could be viewed as a pivot point for 3D printing in pharma, taking the technology out of the lab and into the mass marketplace.
However, the question currently being asked is whether the narrative that is used to describe the impact 3D printing will have on other industries – localised, on-demand production, minimising waste and transport costs, that allows goods to be tailored to the individual – actually applies to pharma.
It is clear that on-demand printing of drugs could tackle a major issue facing pharma companies, namely that stock levels being held by the top 25 companies are estimated to be between $100bn and $150bn at any time, and inventories typically account for half of the overall cost of goods sold.
For the moment, Aprecia is nowhere near talking about locating production in doctor’s offices and is sticking to the usual model in the industry, manufacturing batches of Spritam in pre-defined strengths from its facility in Blue Ash, Ohio, prior to a launch in early 2016.
For now, many of the advances promised by 3D printing remain at the R&D stage, but Spritam’s approval is an endorsement not just of the potential of the technology, but also the willingness of regulators to accept it.
Meanwhile, researchers continue to push the boundaries of 3D printing in formulation science. Scientists from the University of Nottingham in the UK have demonstrated the potential of the polypill by combining three different cardiovascular drugs – the ACE inhibitor captopril, diabetes drug glipizide and calcium antagonist nifedipine – into a single tablet using 3D extrusion-based printing.
The three compounds in the pills – which could potentially be used to treat diabetes with high blood pressure – were shown to behave as expected in the body. The work “is a significant step towards the demonstration and validation of 3D printing for the tailored manufacture of medicines,” said the researchers.
They have since gone a step further by creating a polypill with no fewer than five drug components, all used in patients with cardiovascular diseases such as heart failure: aspirin and the diuretic hydrochlorothiazide in an immediate-release layer, and three sustained release compartments containing pravastatin, atenolol, and ramipril.
In addition to loading multiple drugs into a tablet, 3D printing could also open up the potential of personalised doses, delivering just the amount of active ingredient needed to the patient.
That can be a challenge if the drug has a narrow risk-to-benefit window, for example, or if the patient is a premature infant who needs a tiny dose. One might even argue that the forward strides being made in diagnostics and molecular biology to allow personalised medicines will not be realised without matched advances in drug delivery.
The jury is out as to whether inkjet will ever be suitable for large-scale production
Meanwhile, the compromises taken when drugmakers plump for a particular dose for mass production are well known. For instance, Eli Lilly’s antidepressant Prozac (fluoxetine) was launched in a dose that worked in two-thirds of patients, even though a more than half of patients in trials derived a benefit from a lower dose associated with fewer side effects.
One research team looking at this problem have worked with a particular form of 3D printing called fused deposition modelling (FDM). They have shown that when this technique is used alongside a hot melt extrusion process – already widely used to make tablets – medicines can be printed in a broad range of doses, although it is only usable for drugs that are heat-stable.
As FDM printers are small and low-cost, the approach could potentially be deployed within healthcare facilities for on-demand medicine production, according to the researchers, from University College London and the University of Bradford in the UK.
Other established printing technologies such as inkjet are also being looked at for their pharmaceutical applications, ranging from high-throughput drug discovery to oral dose manufacturing.
While this work is generally in the preliminary stages, thermal inkjet printing has been used to produce pharmaceutical co-crystals – a combination of an API with another compound that improves its bioavailability, stability or ‘processability’ – and also to print drugs directly on to edible polymer films or as a coating on devices such as microneedles or stents.
A team of researchers from the UK, US and Greece recently reported a study in which they printed anticancer medicines on microneedles administered via a patch onto the skin, demonstrating rapid and painless systemic release of the drugs.
A key advantage of inkjet is its scalability – the size of a production operation can be increased simply by adding more print nozzles to the printhead or running multiple printers side-by-side. However, there is an upper limit to the doses that can be printed without clogging, and the jury is out as to whether inkjet will ever be suitable for large-scale production of high-dose drugs.
The vision is that anybody could go to a website, pick their building blocks and instruct their assembly through the web
APIs on demand
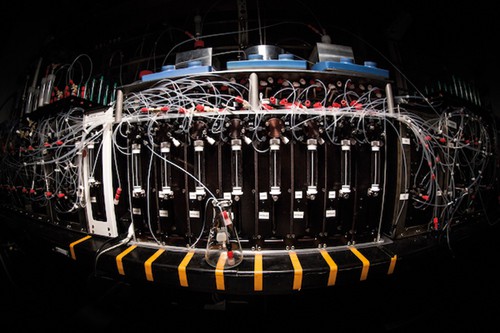
Another key development occurred earlier this year when researchers at the Howard Hughes Medical Institute unveiled a 3D printer that can synthesise 14 different classes of small molecule from a common set of chemical building blocks.
The aim in time is to have enough reagents to allow a user the synthesis of just about any small molecule drug – without any chemical expertise.
Lead researcher Marty Burke said: “the vision is that anybody could go to a website, pick the building blocks they want, instruct their assembly through the web, and the small molecules would get synthesized and shipped.”
It is clear that 3D and 2D printing approaches tie into one emerging trend in the pharma industry – a shift from large-scale batch production to processes based on smaller, continuous manufacturing of stratified or personalised drugs.
The technologies raise a huge number of questions however, not least of which will be the need for sweeping changes to what is considered Good Manufacturing Practice (GMP), including procedures to ensure dose accuracy and sterility and taking into account the possibility of manufacture at the point a drug is dispensed.
Pharma companies will also have their work cut out defending their intellectual property when 3D printers become widely deployed and have the potential to design, synthesise and formulate small-molecule drugs at will.




