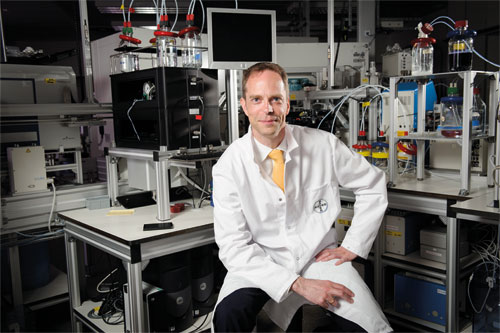
Alex Moscho is no stranger to finding ways to answer difficult organisational and healthcare system questions. At Bayer he had been focused firmly on questions of strategy until his 2014 move to the UK.
The company, like many of its peers, has been working its way through a major programme of organisational change that has recently been coming to fruition.
Now managing director of Bayer UK & Ireland, in his former role within the German firm’s Leverkusen headquarters as head of corporate development he was closely involved in these strategic deliberations.
The question of healthcare systems change is also very much on his mind when we talk, and clearly it’s an important issue from a Bayer perspective. But, with Alex elected chair of UK industry group the European Medicines Group over the summer, he’s increasingly been taking a multi-company view on the issue as the Group represents European pharmaceutical companies that operate in the UK.
Broader understanding
A biotechnologist by training, Alex’s studies combined areas such as biochemistry, biology, medicine and engineering, culminating in a period as a visiting scholar in analytical chemistry at California’s Stanford University.
After working at the intersection of different disciplines in pursuit of medical innovations, he took the decision to broaden his experience and join McKinsey. His role at the consultants provided, he says, valuable insights into how products find their way to patients and markets, as well as a broader understanding of market dynamics – not to mention the range of modern healthcare stakeholders.
“I worked with payer organisations, hospitals, hospital chains, physicians, physician networks and with the pharmaceutical industry. That was something that was really intriguing to me to understand the different elements that come together to form then a sustainable healthcare system,” Alex says.
During this time he worked for two years in the UK and was tasked with finding his way around the challenges inherent in a national healthcare system that’s also the world’s fifth-largest employer. Then, as now, Alex says there were “significant question marks around the sustainability of the NHS overall”.
“That’s obviously an area that is close to our heart as a pharmaceutical company, because we want to help ensure the NHS develops in a way that means it can be sustained over the long term.”
It’s a challenge that is not, of course, restricted to a single local market in this region. “What we see across Europe is basically publically-funded healthcare systems trying to bridge the challenge between the limited amounts of funding made available and increasing financial requirements to support the services needed for patients in those systems,” Alex says. “Most importantly, this challenge will not be solved by focusing on costs for medicines, only, which constitute just 10% of all costs of healthcare.” But, turning back to the UK, he says the country “still has a way to go”, even when compared to its neighbours.
[There are] significant questions marks around the sustainability of the NHS
Representing European pharma in the UK
Set up in 2001, the European Medicines Group (EMG) provides a voice on health and industrial policy issues for the UK operations of pharma firms with headquarters in continental Europe. Its 18 member companies include Sanofi, Novartis, Roche, Boehringer Ingelheim and, of course, Bayer. Taken together, these firms supply around a third of all the medicines prescribed by the NHS.
Over the summer Alex was appointed chair of the EMG, taking over from Merck’ Serono’s David Garmon-Jones, and he says both the EMG and its wider, UK industry counterpart the ABPI, provide very open forums for constructive discussions about how the pharma industry can contribute to health and healthcare in the UK and the decisions society need to make on what is prioritised.
When it comes to the EMG Alex says the body certainly has something to bring beyond to the table, to augment what ABPI does on a broader basis. He explains: “EMG has a fairly tight focus – on patients access to innovative medicines and how the UK compares to similar countries in Europe. We know very well where the European healthcare system stands, how things work, how innovation is drawn to patients across many other European countries, and as the systems across Europe have some striking similarities.”
He adds: “There are a lot of insights and learnings that we, as European headquartered pharma companies, can bring from our experiences also to the discussions here in the UK.”
From strategy to operations
Alex’s path to the EMG chair began when he assumed his current role as CEO for Bayer UK and Ireland in February 2014. Having moved from McKinsey to Bayer in 2006, prior to his UK move he held a number of roles, including leading on corporate strategy portfolio development for Bayer’s global operations, based at its German headquarters in Leverkusen.
The company’s corporate strategy has gone through a period of change. In September the move to carve out its polymers business, Bayer MaterialScience, as a separate entity was completed, and that now operates as an independent stock listed company under the name Covestro. And that’s not the only change from where the Bayer of today differs from where the firm was some 12-18 months ago.
While focusing on LifeSciences, Bayer was working hard to boost its standing in the consumer health space. In May 2014 it paid $14.2bn for Merck & Co’s consumer health unit. This was followed five months later by the smaller, but still notable, deal to acquire the Chinese consumer healthcare company Dihon Pharmaceutical for around $485m.
These moves were followed by Bayer’s announcement to focus on health of humans, animals and plants reflected by the company’s realignment into three divisions, pharmaceuticals, consumer health and crop science – changes that are scheduled to take effect from January.
“I was part of designing this journey in my previous role,” Alex says, “and had the privilege to support the Board in preparing the strategy that ultimately led up to where we are today.”
Everyone’s challenge
Alex’s current role has given him a front-row seat for the challenges of the UK pharma market, particularly those of access and working with NICE and the variations in access within the different parts of the UK.
This is often most notable when Scotland’s SMC takes a different opinion on a new drug from its counterpart for England and Wales, NICE. ‘Medical apartheid’ was a particularly forthright interpretation of the situation from one UK newspaper when NICE rejected Janssen’s Velcade in 2006.
Nevertheless, the UK’s north-south differences are well known, as a 2012 study of the two health technology assessment (HTA) bodies confirmed. Looking at rulings in the decade to 2010 it found that NICE and the SMC held the same view on the availability of drugs in 71% of cases – with the remainder being split between different restrictions being required (18%) and a different outcome from their appraisers (11%).
“Many other European countries are much better equipped to enable their patients’ early access to innovative therapies. And that’s something that we want to change and where we want to build on learnings from our neighbours.”
But he adds: “It’s not just a challenge that the UK pharmaceutical industry is facing – it’s basically a challenge for every person living in the UK, who don’t get the same level of access that you get in other countries in Europe.”
We see a lot of potential for the Cancer Drugs Fund to evolve
He acknowledges that the Institute has had its successes – with its methods exported to other countries and widely-respected. But he adds that NICE – now not far off its second decade of operations – hasn’t kept pace with healthcare systems changes and characteristics of innovative medicines.
“The challenges that the whole system – including the industry – faces, and the options we offer patients, have evolved significantly since the early days of NICE. Yet it has not evolved on the same level and with the same speed, and where we would support NICE today would be basically in their next evolution, which should reflect appropriate approaches to the more complex and broader treatment options that patients find with regard to medicines.”
The timeline for such changes is difficult to gauge, which is frustrating for the industry – NICE recommendations are still hugely important when it comes to improving patient access to new medicines, though still no silver bullet. Nevertheless, the alternative for companies marketing a non-NICE considered drug in the UK can be going through over 200 local-level assessments which often results in different funding decisions in different parts of the country.
The UK’s ring-fenced oncology budget is another bone of contention for many in pharma (not to mention the wider healthcare ecosystem). Set up in 2011 and only intended as a stop-gap measure, the demands on Cancer Drugs Fund (CDF) have grown over the years with it now running over the original budget and was recently pronounced ‘unsustainable’ by the National Audit Office. Proposed reforms that would see it act as a ‘managed access’ fund with closer integration with NICE have been put out for consultation, though whatever the outcome of these the CDF is likely to continue offering a special pass for oncology drugs, with no signs of other – no less deserving – therapy areas receiving such treatment.
“We see a lot of potential for the Cancer Drugs Fund to evolve, and I would hope that it paves the way for more creative thinking about how to solve access issues across all therapy areas so that there are appropriate approaches to consider the value of all medicines and society gets a healthcare system which funds and provides treatments that we would all expect as standard in a country such as the UK” notes Alex.
He adds: “We must ensure all stakeholders in the system, including patients and their organisations, are part of this discussion. As an EMG member, as a representative from Bayer and also as a person living in the UK, it is crucial that we find a good way to move from an oncology solution to ensuring that the healthcare system develops to drive access and uptake of innovative medicines in all disease areas.”
Deliberations on the future of the CDF, NICE and access are certainly difficult questions, but they’re vital ones for all healthcare stakeholders to find sustainable solutions to for the good of patients. Alex concludes: “The reason I joined the pharmaceutical industry is because I believe in its ‘value-add’ and the contributions that we bring to healthcare systems and patients. Obviously, we can do this only if we find a sustainable way for healthcare systems to work.”




