
Having reached its 70th birthday earlier this year, do you think the NHS will be able to adapt and thrive in the coming decades?
Pfizer is proud to have worked alongside the NHS supplying medicines for over six decades to support the provision of high-quality healthcare to everyone that is free at the point of use. We are also acutely aware that the health service is at a critical juncture and is under immense pressure due to the realities of an ageing population and the burden of chronic diseases, as well as advances in treatment and technology.
We are committed to working with the NHS in a new partnership to achieve the best health outcomes for people in the UK. But we must find new ways to embrace next-generation ideas and technologies that can transform care and improve lives, within the constraints of limited resources.
We are already supporting the NHS to understand how emerging technologies, such as artificial intelligence, can help patients and alleviate the strain on healthcare services and it is partnerships like these which will help to sustain the NHS.
The Life Sciences Industrial Strategy could increase the speed with which new medicines and vaccines are made available across the UK, if implemented in full and with the involvement and commitment of the NHS.
It is therefore essential that strategic planning for introduction of transformative technologies including medicines is a key pillar of the ten-year strategic NHS plan. Likewise, a new voluntary scheme agreed with the Department of Health and Social Care could provide an opportunity for the Government and industry to anchor solutions into upcoming plans and policies. The current scheme has seen pharmaceutical companies contribute more than £2.8bn to the Government to help support a sustainable NHS.
Other European healthcare systems are often compared favourably to the NHS, such as that in your native Netherlands. How do you think those two compare?
While comparisons of different countries’ health systems are difficult, they do provide an important perspective on what the NHS does well and where it could potentially improve.
It’s important to flag that I haven’t worked in the Netherlands for 25 years, so my knowledge of the healthcare system isn’t what it once was! However, my brother is an orthopaedic surgeon and regularly updates me on important developments from a clinical perspective.
The most obvious difference is that the Dutch have health insurance, and so healthcare is mostly handled through a handful of private providers. When you add this to a history of more central planning for healthcare, it means that there is more consistency in the way healthcare is delivered. In addition, following major reform in 2006, management of the system is largely the responsibility of relatively independent bodies rather than the government.
The Netherlands has one of the highest healthcare spends in Europe. 10.8% of GDP is spent on healthcare in the Netherlands versus 9.8% in the UK.
Since the Netherlands is among the five wealthiest countries in the eurozone, the Dutch have high expectations. In two recent surveys, 91% of Dutch people evaluated the quality of the health system as good whereas only 60% of British people said they were either satisfied or very satisfied with the NHS.
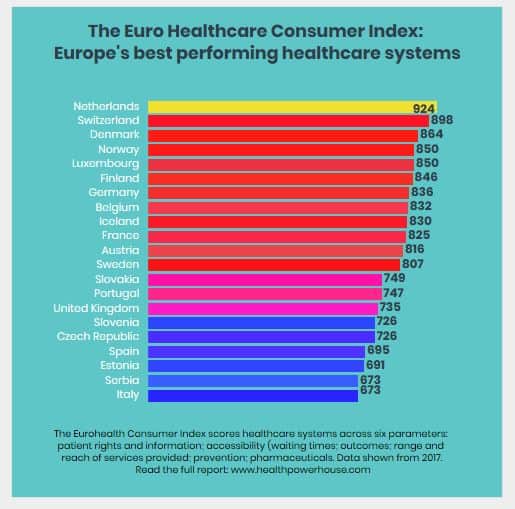
Interestingly, the Netherlands has secured the number one spot in the Euro Healthcare Consumer Index for at least the last six years. This compares the performance of national healthcare systems in 35 countries and ranked the UK number 15 in 2017. The position that the Netherlands enjoys may be due to the fact that essential healthcare services are within easy reach and waiting times meet national standards in most cases. The Netherlands also has probably the best and most structured arrangement for patient organisation participation in healthcare decision – and policymaking in Europe.
Finally, the Netherlands usually appears within the top five when it comes to outcomes results whereas the UK often features close to the bottom.
While the two healthcare systems are clearly different, I do think that there are learnings the UK can take from the Netherlands, particularly with regards to investment and access.
Our health system is at a pivotal point and we have a once in a generation opportunity to deliver an NHS that’s truly fit for the future.
Brexit, the Industrial Strategy, the new pharmaceutical price regulation scheme and the recently announced long-term funding settlement for the NHS all present opportunities.
You’ve had direct experience of lots of other healthcare systems – what can the NHS learn from some of the best examples?
I’ve had the privilege of working in Belgium, Germany and Greece, as well as in the UK. Since most European countries are experiencing similar pressures, it’s useful to assess the different healthcare systems and the ways these issues are being managed while acknowledging the limitations associated with such comparisons.
Belgium and Germany often appear near the top of international league tables when it comes to health. Both countries’ healthcare systems are funded through social insurance contributions rather than general taxation and in both instances the state plays less of a regulatory role than in the UK.
Health spending in Belgium and Germany is around 10.4% and 11.1% of GDP respectively, which is higher than the EU average of 9.9% and the UK average of 9.8%. The two countries have restructured healthcare in recent years to help sustain the system and Belgian and German patients alike enjoy good access to quality health services. However, while Belgian satisfaction scores are high, German satisfaction scores are low suggesting improvement is needed in certain areas, particularly quality of treatment.
The situation in Belgium is especially interesting right now. Historically, the country has been a fertile ground for pharmaceutical innovation and steps have been taken recently to consolidate and strengthen its leadership position with regards to clinical trials.
In 2015, Health Minister Maggie De Block entered into a mutually beneficial agreement with the pharmaceutical industry to ensure that patients continue to benefit from the best medical care and that medicines continue to meet the highest quality standards. Known as the Pact for the Future, it aims to improve access to medicines for patients, foster innovation within the industry and provide a new ethical framework for the sector as a whole. The agreement also offers the industry perspective and predictability and, at the same time, encourages the industry to contribute to efforts at budget control.
Unfortunately, my time in Greece coincided with the height of the country’s economic crisis, which understandably severely affected healthcare spending. Since 2009, per capita spending on public health has been cut by nearly a third, thousands of healthcare workers have been made redundant and critical hospital supplies often run out.
As a consequence, Greece is a country that has gone from a country that was an eager and early adopter of novel pharmaceuticals to one that has unsurprisingly become much more restrictive. During the most difficult times, politicians had to choose where they took the pain within a severely constrained budget, but they always prioritised healthcare and access to the most innovative medicines relative to other areas.
Lastly, is there really a breakthrough happening in NHS-pharma partnerships? Can you give me some examples?
Our health system is at a pivotal point and we have a once in a generation opportunity to deliver an NHS that’s truly fit for the future. Brexit, the Industrial Strategy, the new pharmaceutical price regulation scheme and the recently announced long-term funding settlement for the NHS all present opportunities.
However, a fundamental shift is required towards greater partnership, between the Government, the NHS and the pharmaceutical industry so that we can ensure that everyone benefits from the wave of transformative technologies in the healthcare sector. Both in terms of productivity gains, healthcare outcomes, and patient and healthcare professional experience.
Companies like Pfizer can and want to provide much more value to the NHS by offering new approaches to service delivery that generate real and tangible efficiencies that we plan for and can be easily executed.
An example is EPIFFANY (Effective Performance Insight for the Future) – a number of collaborations between healthcare organisations in the East Midlands and Pfizer. This is an educational approach for junior doctors and is designed to increase patient safety and reduce human error by improving prescribing confidence, competence, performance and attitudes towards safe prescribing and patient care.
In 2013, the initial pilot site at the Renal Unit within Leicester General Hospital, which was supported through an educational grant provided by Pfizer, reported an increase in prescribing competence using the EPIFFANY educational approach.
The University Hospitals of Leicester NHS Trust reported that for the renal unit concerned, this translated into a 50% reduction in prescribing errors over a four-month period, with a potential cost avoided estimated to be approximately £300,000 and a potential of 489 bed days avoided.
We have also joined forces with Swansea University and the emergent Llanelli Wellness and Life Science Villages Consortium on real- world research and innovation projects in the health and life sciences sector, to support and drive towards the vision of delivering improved health and well-being for the region’s population of approximately 1 million people.
Although primarily focusing on South Wales, we firmly believe that the outcomes from our partnership with Swansea University will have application far beyond the region.
With the UK-wide healthcare system facing rising demand for high-quality care it is important new and innovative ways are considered to improve system efficiency and get the best value out of medicines. We believe that by combining our skills, experience and resources, we can work towards delivering better patient care, improving patient outcomes, saving the NHS money and speeding up patient access to new health innovation.




