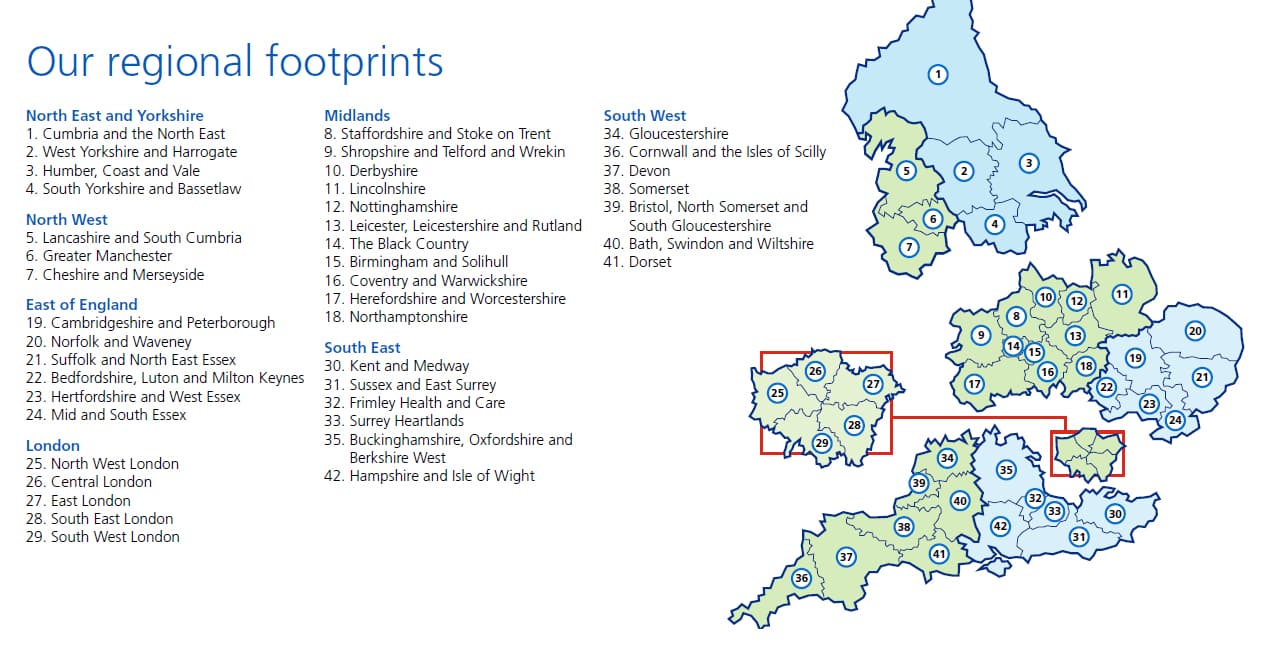
Towards the end of 2018, a map was published by NHS England (NHSE) and NHS Improvement (NHSI), which divided the country into 42 ‘regional footprints’ responsible for delivering health and social care services.
Regional footprints are NHSE and NHSI regional offices. They align with Sustainability and Transformation Partnerships (STPs) and Integrated Care Systems (ICSs) to support integrated working, particularly around organisational control totals and long-term budgeting.
Within the footprints, Clinical Commissioning Groups (CCGs) are playing an increasingly strategic role in statutory decision-making for integrated care, while providers within ICSs focus on service redesign. This article looks at how the NHS integrated care delivery picture is changing, what this means for pharma and how pharma should navigate the integrated care landscape in 2019.
Integrated care units
Fourteen areas in England have been given the green light to become ICSs, which see one provider or a group of providers responsible for all the health and social care needs of a defined population in order to improve outcomes and reduce costs. ICSs have been tasked with re- designing services around patients’ needs, both within hospitals and also across primary care, which encompasses all health and social care services that are not provided within hospitals. Key objectives include providing more joined-up care closer to patients’ homes and reducing hospital admissions.
A variety of service providers, such as acute and community Trusts, mental health, ambulance services and social care, are currently working together on the redesign of services within ICSs. However, many ICSs are waiting for a proposed change in legislation in 2019 which would give their providers statutory powers and enable them to operate as a single entity.
While the integration agenda is led strategically by the ICSs and STPs, the local operational delivery vehicles for these organisations are the new neighbourhoods of care, which are responsible for populations of around 30,000-50,000, about the same reach as a large supermarket. In neighbourhoods, all services – police, health and social care – work together more holistically.
They are based around primary care networks which are the health element of the provision and include services from community, mental health, the third sector and even acute Trusts as well as GP federations.
CCGs take leading role
To enable larger-scale commissioning within STP areas and to help pave the way for the creation of ICSs, many CCGs have merged in recent years. In some localities like greater Manchester these CCGs already mirror the STP and they will form the organisations responsible for strategic commissioning, which is concerned with meeting outcomes within a whole population budget.
In these areas, the traditional function of the CCG has been redefined and they are playing an increasingly strategic role in statutory decision- making for place-based care. This style of working is expected to widen across the country, with CCGs being responsible for buying services from integrated care providers, managing their delivery and overseeing the work of the service providers.
The widening role of CCGs was underlined by the recent paper, CCG Improvement and Assessment Framework 2018/19, published by NHSE, which acknowledged CCGs as ‘local system leaders’. It said: ‘To ask CCGs to focus solely on what resides exclusively within their own organisational locus would miss out what many are doing, and artificially limit their influence and relevance as local system leaders.’
The framework also outlined some new performance indicators for CCGs for 2018-19 that are relevant to integrated care, including the proportion of people on GP severe mental illness registers receiving physical health checks in primary care and the number of patients waiting six weeks or more for a diagnostic test.
 CCGs in action
CCGs in action
In Nottinghamshire, six CCGs have joined forces to lead the strategic development of integrated care within the geographical area originally allocated to the Nottinghamshire ICS. The CCG is starting to take responsibility for bringing services out of hospitals and into the community, which is a key NHS priority. For example, the CCG has contracted services for musculoskeletal disorders (MSK), from the Nottinghamshire Integrated Care Partnership (ICP), which is now delivering services around rheumatology, arthritis, physiotherapy, imaging, primary care management, biologics and joint replacement. It is combining them with a triage system for all patients and elements of social care.
In the south-west of England, the NHS Dorset CCG, which is the commissioning organisation for the whole county, has been working with the NHS and local authority organisations and consulting with the public on improving patient services. Plans include significant changes to the way acute, GP and community-based healthcare services are provided.
For example, it was decided that the Royal Bournemouth Hospital would become a major emergency hospital while Poole Hospital would become a major planned care hospital. Dorset County Hospital would continue to provide emergency and planned services to meet the needs of people living in the west of the county. The CCG also wants to commission community hubs – some with beds and some without – in a number of hospitals in order to bring care closer to patients’ homes.
While there are common themes running through the above examples in terms of bringing care closer to patients’ homes and integrating health and social care services, each of the 42 footprints will have different local challenges and different ways of providing ‘placed-based care’. Pharma must keep abreast of the needs and priorities of each regional footprint. Digital tools are key to managing this in a timely and efficient way. For example, Wilmington Healthcare’s Healthcare Transformation Tracker enables pharma to search lengthy NHS documents at the touch of a button to identify opportunities within specific regions and allocate resources appropriately.
Reducing whole system costs
The importance of delivering value across the whole patient care pathway was underlined in the recent announcement of a ‘new integrated oversight framework’ that is under development for ICSs and STPs. While NHS Improvement and NHS England will continue to look at Trust level and CCG level data, it was stated that the new framework ‘will… reflect a population-based approach to improving health outcomes and reducing health inequalities’. The regulators said this would provide ‘greater focus on the performance of the local healthcare system as a whole’.
Pharma must ensure that it looks beyond the cost and efficiency of treatment at a single point in the care pathway and thinks instead about the whole care pathway. So, for example, what are the implications of failure rates for a drug? What are the implications of changing the care pathway further down the line due to a reduction in side effects from a medication? In line with this, pharma needs to understand market segmentation for its products to identify where and how they offer best value.
NHS RightCare, which has defined optimal care pathways across wide-ranging therapy areas, provides useful examples of integrated care in practice. The methodology used by Getting It Right First Time (GIRFT), which is reviewing around 40 surgical and medical specialties to reduce unwarranted variation in care, also provides valuable evidence for pharma companies looking to understand how the NHS aims to get better value for money and improve patient outcomes. There is also a role for pharma to play in educating clinicians about transformational change that is happening in their area, the implications of it and why a potentially transformative new product or service is needed. Industry must also engage more widely and potentially find ways to educate the variety of stakeholders now involved in regional footprints, where local authority officers, pharmacists, the third sector and patient groups have become increasingly influential.
Conclusion
In 2019, we expect to see more CCGs playing a strategic role in the development of the 42 regional footprints as the theory of place-based, integrated care models is put into practice across England. The way in which these footprints will design and deliver services will vary according to local needs and priorities.
However, the end goal is to save money across the whole care pathway by providing more efficient, joined-up services that improve patient outcomes. Pharma needs to understand this overarching picture and think holistically across the whole care pathway to define how and where its products will fit in. In line with this, it needs to educate clinicians about the wider value of its products within the integrated care agenda and find ways to engage with the variety of other key stakeholders who are bringing their influence to bear within regional footprints.




