Skin cancer drugs Yervoy and Zelboraf should soon be available for mainstream use on the NHS in England and Wales after the National Institute for Health and Clinical Excellence (NICE) agreed a discount with both of the drug’s manufacturers.
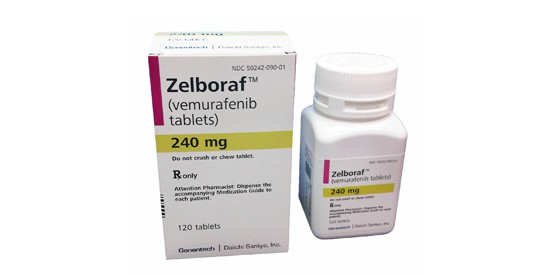
The final draft guidance from NICE recommends Bristol-Myers Squibb’s Yervoy (ipilimumab) for the treatment of advanced malignant melanoma in people who have received prior chemotherapy, while Roche’s personalised cancer drug Zelboraf (vemurafenib) is recommended for the treatment of unresectable locally advanced or metastatic melanoma in patients who have the BRAF V600 mutation.
Both treatments will only be available under separate patient access schemes, however, which will see Roche and BMS cover part of the cost of their respective treatments. The size of the discount involved in both schemes remains confidential.
The recommendations come after an uncertain journey through NICE assessment for both drugs, with previous draft guidance raising concerns over their cost-effectiveness.
NICE initially failed to recommend Zelboraf in its first draft guidance, released in June, 2012, stating that more information was needed regarding the drug’s long-term survival prospects, and that a larger patient access scheme was necessary.
At the time this caused Roche UK’s managing director John Melville to comment “the use of the existing NICE methodology highlights a need for change in order for value-based pricing to meet the government’s stated access to medicines objectives”.
Second draft guidance, released in August, 2012, also did not recommend the drug, with NICE once again demanding further analysis from Roche to justify the drug’s “significant cost”.
Despite these concerns over its price, Zelboraf has been available in the UK since March, 2012, through the cancer drugs fund – an annual fund of £200m to pay for cancer drugs that do not have a NICE recommendation.
However, this fund is set to close in March, 2014, once a new value-based system of drug pricing has been implemented, and Roche welcome NICE’s latest recommendation to allow the drug’s continued use.
“Today is a landmark day for metastatic melanoma patients who will now have access to Zelboraf, a treatment that extends and improves quality of life,” said Melville.
“All patients should now be tested to see if they are BRAF mutation positive in order to determine eligibility for treatment with this personalised medicine.”
A Roche spokesperson also provided an update to PMLiVE regarding Melville’s concerns with NICE’s methodology.
They said: “The decision to grant access to an end-of-life medicine in an area of high unmet need and clinical innovation instills confidence in the system, however many oncology medicines are not granted approval by NICE. Roche hopes that the pending value-based pricing system will ensure access to cancer medicines in the future.”
The antibody Yervoy faced similar troubles getting through NICE, with the Institute releasing draft guidance in October, 2011, claiming BMS’ drug, which costs around £80,000 per patient, was not a cost-effective option based on available data.
The patient access scheme offered by that pharma company appears to have caused NICE to reconsider, however, meaning patients in England and Wales will have access to the drug.
Professor Carole Longson, health technology evaluation centre director at NICE, said: “These new draft recommendations represent really good news for skin cancer patients.
“Vemurafenib and ipilimumab are breakthrough treatments that can potentially significantly affect prognosis for these patients and we are very pleased that the manufacturers have worked with us so that we are now able to recommend both ipilimumab and vemurafenib.”
Gill Nuttall of patient support group Factor 50 added: “I am absolutely delighted that NICE have overturned their original decision and that the patients I speak to every day can start to get the treatments that they so desperately need.”




