A new study from the Department of Biology at the University of Oxford has found the first direct evidence of antibiotic resistant bacteria migrating from a patient’s gut microbiome to the lungs.
The findings suggest that eliminating antimicrobial resistant (AMR) pathogens from the gut microbiome of hospitalised patients could help prevent serious infections, and highlights how antibiotic use can have ‘profound impacts’ on bacteria that are not actually the target of antibiotic treatment.
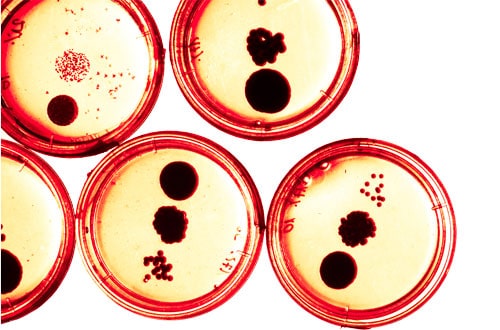
The study, published in Nature Communications, was conducted on a patient that carried the bacterium – a Gram-negative bacterium that is one of the leading causes of infections in hospitals, and one that is particularly good at resisting antibiotics – as part of their gut microbiome.
While Pseudomonas is generally not considered to be dangerous when it is embedded in a healthy gut microbiome, it can cause serious infections in the lungs of hospitalised patients.
The patient was treated with the antibiotic Meropenem for a suspected urinary tract infection, which caused non-resistant bacteria in the gut and lung to be killed off, and antibiotic resistant mutants of Pseudomonas to grow and proliferate.
The researchers then found Pseudomonas was able to translocate from the gut to the patient’s lungs during antibiotic treatment, where it evolved even higher levels of antibiotic resistance.
AMR develops when bacteria, viruses, fungi and parasites change and adapt to antibiotics over time, making them more resistant to drug treatments. As a result, infections become harder to treat and the risk of severe illness and death increases.
The World Health Organization reports that AMR is one of the top ten threats to global health, causing 1.3 million deaths in 2019 alone from bacterial AMR.
“There is a clear need to develop new approaches to the challenges that antimicrobial resistance presents,” said Professor Craig MacLean, professor at the Department of Biology.
He continued: “Our study shows how gut-lung translocation and antibiotic use can combine to drive the spread of AMR within a single patient. Insights such as this are needed in order to develop new interventions to prevent resistant infections.”
Following on from the study, the researchers plan to assess how frequently gut to lung bacterial translocation occurs in vulnerable patients by collecting samples from a much larger cohort.




