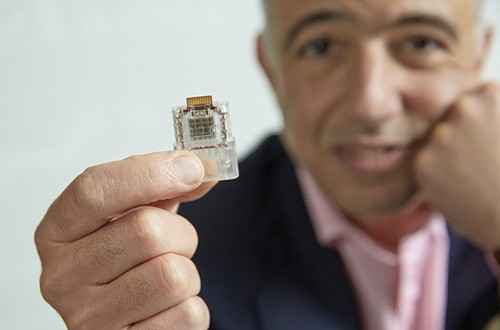
Chris Toumazou, DNA Electronics
With a few notable exceptions – such as the alarmingly expanding screen sizes for smartphones – technical advances typically go hand-in-hand with miniaturisation.
Laboratory science is no exception and for some time researchers have been developing new analytical devices that cram the equipment and reagents used in modern biology and chemistry labs onto tiny devices, the size of microchips, that can conduct hundreds of reactions in parallel.
The secret to these ‘lab-on-a chip’ devices – so called because they grew out of fabrication technologies developed by the microelectronics industry – is the principle of microfluidics, which essentially means the controlled manipulation of volumes of liquids or gases on a minute (micrometre) scale.
Liquids can be carefully guided through a labyrinth of microchannels housing a series of nanoscale chemical, physical and biological tests to answer a plethora of scientific and clinical questions.
It sounds like the stuff of science fiction, but microfluidic devices are already being put to use in the pharmaceutical industry in areas such as drug discovery, for example by allowing thousands of compounds to be screened against a drug target such as an ion channel or to check the profile of proteins expressed by a cell.
Genetically, we all differ by 0.1%, and it is that 0.1% difference … that my microchip is trying to detect
Chris Toumazou
The devices – sometime called micro total analytical systems or μTAS – can perform tasks such as mixing, reacting, product formation, separations and dilutions, assays and removal of waste materials, all within within a single unit. Add multiple μTAS units together, and the potential for sophisticated reaction and analytical pathways becomes clear.
For example, one of the most challenging tasks in drug discovery is predicting pharmacokinetic behaviour in humans, but microfluidic devices are now starting to be used to recreate cell-cell interactions in simple organ systems and give a truer picture of how drugs will behave in the body.
Chips have now been developed that mimic the blood brain barrier in humans and can be used to test whether a drug is suitable for central nervous system disorders, and to make functional blood vessels that can be used to test drugs for endothelial activity. Just recently, researchers from the University of Toronto in Canada have used microfluidics to develop ‘liver organoids’, free-floating clumps of various cells found in the liver that can be used to test the safety of pharmaceutical compounds.
Even for a relatively simple procedure such as high-throughput screening, the advantages are manyfold compared to traditional techniques. Microfluidic devices are quicker, use fewer sample and reagent volumes and can even tap into the unique physical properties of microscale fluid flow, such as high surface-to-volume ratios, small diffusion distances and surface tension that may sometimes be more representative of the environment within the body.
The number of companies developing microfluidics devices for drug discovery applications is still fairly small – including the likes of Caliper, Gyros, Cellectricon, Fluidigm and Nanostream – but rapid advances in the technology underpinning the devices means that in some respects the field is fairly mature.
In the area of diagnostics, however, the story is still largely one of future promise rather than present reality, although some microfluidic devices have made it into the point-of-care (PoC) diagnostics setting.
Once again, the premise is compelling. Rather than take a blood sample, send it off to a centralised lab for analysis and wait days or weeks for the results, lab-on-a-chip technology could allow diagnosis to be carried out using a drop of blood in the doctor’s office in minutes, with rapid detection of a range of biological entities including cells, bacteria, proteins and DNA.
A recently published report by microelectronics market specialist Yole Développement suggests PoC testing based on microfluidic technology was already a $1.6bn market in 2013 – depending on the definition of the term – and will grow rapidly to reach $5.6bn in 2019.
Major diagnostics companies such as Alere, Abbott, BD Diagnostics, Cepheid and Abaxis have started to realise the potential of rapid molecular diagnostic testing and are making inroads into the market.
Access to microfluidic technologies for diagnostic companies has generally come about through acquisitions, says Yole, as this reduces the technology development risk and increases reactivity. The most recent acquisition was that of IQuum by Roche for $450m in April, which gave it access to the Laboratory-in-a-tube (Liat) system which automatically executes all the required assay processes, including reagent preparation, nucleic acid purification, amplification and real-time detection.

Several other successful PoC products based on microfluidic technology have been launched in the past few years. Good examples include Abbott’s i-STAT cartridges, which can carry out a battery of clinical tests – including cardiac markers, lactate, coagulation, blood gases, chemistries and electrolytes, and haematology – and Agilent’s HPLC-chip range for the analysis of DNA, RNA, proteins and cells using mass spectrometry.
While routine use of these devices in the doctor’s office is still rare, there are some tantalising signs that the field is gathering momentum. Earlier this year, Chris Toumazou – the head of firm DNA Electronics which focuses almost entirely on microfluidics-based DNA testing – was awarded the European Patent Office (EPO) European Inventor Award 2014 in the research category for a rapid diagnostics device that plugs into a USB port.
The unit, which can provide the results of a DNA test within 20 minutes, uses silicon transistors to identify DNA and RNA, offering a simpler, cheaper and more discrete alternative to existing DNA analysis equipment. It is so simple that patients can even run the tests themselves, says Toumazou.
“Genetically, we all differ by 0.1%, and it is that 0.1% difference … that my microchip is trying to detect,” he explains. “It is those differences that tell us whether or not we can metabolise drugs differently or whether we have different genetic diseases.”
The amount of research papers being published in this area is also rising fast. To give just a couple of recent examples, researchers at Stanford University of Medicine in the US have just developed an inexpensive, portable, microchip-based test for distinguishing between the two main types of type 1 diabetes, providing an alternative to an expensive, lab-based test for the autoantibodies that characterise the disease that currently requires specialist radiofacilities.
Meanwhile, a team from Simon Fraser University has developed a microfluidic device that can detect proteins that contribute to multidrug resistance in acute myeloid leukaemia using a single cell harvested from liquid biopsy samples, and could be used to monitor patients undergoing chemotherapy. Other teams are trying to do away with biopsies altogether by using lab-on-a-chip devices to detect circulating tumour cells in the blood.
Smart medical devices
Aside from the use of lab-on-a-chip devices for diagnostics, early work is starting to point to the potential of incorporating them into smart drug delivery systems that will allow exquisite control of therapy based on ‘reading’ the physiological state of a patient’s body using biomarkers.
Microfluidics is also being deployed directly in the drug delivery sector via the use of devices such as microneedles and micropumps, which have been around for years but are latterly gaining traction thanks to improvements in materials science and microfabrication techniques that have made them more biocompatible and robust. Work is already underway on an implantable microvalve device that could act as an artificial pancreas, releasing controlled levels of insulin which it senses a change in blood glucose levels.
Microfluidic devices – such as the aforementioned blood vessel chip – could potentially be used alongside techniques such as 3D printing with biomaterials to develop engineered tissues for transplantation.
Overall, the potential of the technology is only really bounded by the limits of human imagination and ethics, and companies are now stepping forward to develop the tools to bring new applications to fruition.
For example, Microfluidic ChipShop of Germany has developed a series of functional microfluidic modules that can be joined together like Lego blocks to generate devices scientists can use for proof-of-concept experiments.
The company’s chief executive Holger Becker said recently that microfluidics “has developed from a ‘technology looking for a problem’ to a true enabling technology in almost any new product development in diagnostics and the life sciences.”
“However the development process is still characterised by complexity which translates into long development times, residual technological risk and resulting cost,” he added.




