Does your medical education drive change in clinical practice?
October 18, 2013 | Lucid, Strategic planning, medical education
How to advance outcomes for patients using a medical education process, by Jan Steele PhD, operations director, Lucid
There is a growing body of evidence (eg Bauchner et al, 2001) that standard Continuing Medical Education (CME) activities, where healthcare professionals attend a one-day meeting or similar, do not result in a change in clinical behaviour. This is hardly surprising! Psychologists who study how people change their behaviour describe change as a journey. The change journey has three distinct phases:
- Predisposing: this identifies people ready for change and begins to highlight the gap in their care that the training will address.
- Enabling: this ensures that any intervention (eg lecture, workshop) addresses benefits and barriers to change, allowing peers to work together to understand how they can make the change. It also identifies tools that participants can use to help them make the change when they are back in their clinics.
- Reinforcing: this is a planned intervention where participants are reminded of the need to make the change and are encouraged to share their experiences. It keeps the education front of mind (see figure 1).
Putting theory into practice
Imagine there is new evidence which suggests that accurately determining disease severity at diagnosis in patients with psoriasis improves patient outcomes, as the most effective therapies can be used from the outset. You might plan a meeting designed to support clinical leads in making this change in their department.
Predisposing delegates prior to education
Your aim here is to highlight to the participant the need for a change in clinical practice which will advance patient outcomes. There are several ways to identify a gap between what should be happening and what is actually happening. In the example above, we could ask participating clinicians to:
- Audit newly diagnosed patients to see if disease severity was assessed at diagnosis
- Ask their team to review the charts of the last ten patients they diagnosed counting the number of patients who had their disease severity accurately measured
- Survey their team and ask them how often they think they measure disease severity accurately
- Work through case vignettes to measure how often they would measure disease severity or treat with a certain class of therapies
- Survey patients attending their clinic asking how often they have their disease severity measured.
None of the above is perfect, and the list is not exhaustive, but raising a participant’s consciousness about the need to change before he comes to an educational event makes him more receptive to the education delivered.
Enabling delegates during the education
Plenary talks do not change behaviour, and so the first rule in changing participant behaviour is to make the education interactive. This can include:
- Workshops
- Live interviews
- Case-based teaching and role play
- Debates
- Use of audio-visual aids eg holograms.
It is also critical that you enable your participants to discuss the benefits of making the change and the barriers they perceive (preferably with someone who has already changed their practice). Finally, think about tools and tips that participants can take away to help them change when they return to their clinic.
Reinforcing the change in behaviour
This is regularly overlooked. The participant returns to his clinic and slips back into his old habits. There are various ways of reinforcing behaviour change such as:
- Email messages to the participant from the faculty
- Sharing new data demonstrating that changing practice will advance patient outcomes
- Requesting feedback from the participant to understand how easy the change has been to implement
- Sending case vignettes or self-assessment questions
- Conducting a follow-up audit or survey.
While there is a growing body of evidence that the way we educate needs to change, we still deliver one-day, plenary-heavy meetings. As an industry, if we want to support education that advances outcomes for patients we need to look at education more holistically, and support participants for the entire journey.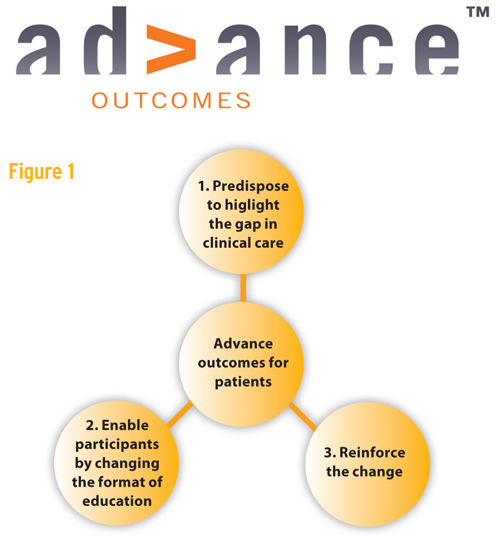
This content was provided by Lucid Group Communications Limited
Company Details
Latest Content from Lucid Group Communications Limited
Lucid Group support local charity event
Lucid Group donated 75 Easter chocolate bunnies to a group of local school children organising an Easter Egg Hunt who were raising funds for Médecins Sans Frontières. The egg hunt...
Why health psychology should inform pharma strategy
In the March 2016 edition of PME, Ella Nuttall (Health Psychology Specialist at Lucid Group) discusses why pharma should look to health psychology and adopt a behaviour-change strategy to inform...
Lucid Group celebrate 9 years of changing patients’ lives
Lucid Group had fun and games celebrating their nine year anniversary in their London offices last week. Lucid has grown from the two founders working out of a basement to...
It's time to get with the real world
Lucid CEO discusses the increasing importance placed on real-world data to demonstrate value
A Lucid Induction
Lucid Group kick off 2016 with six new employees
Lucid’s digital responsibility: delivering value by improving patient outcomes
Digital initiatives must address your customer's needs
Lucid Group US: moving on up!
New premises for Lucid Group US
Lucid group celebrate their outstanding year in style at The Shard
A fabulous montage from our end of year meeting at The Shard. Celebrating our achievements the Lucid way.
Lucid group celebrate outstanding year in style
A well-deserved celebration
Lucid team : because you're worth it!
Lucid group reward the team for an amazing year





