Last month two new reports were published and launched in the British Parliament that both came to the same conclusion: England’s drug pricing watchdog NICE is slowing down access to new medicines – notably cancer treatments – when compared to the rest of Europe.
The reports, written by both IMS Informatics and Abacus International and paid for by Janssen, also found that NICE’s quality-adjusted life years (QALY) formula for assessing the cost-effectiveness of new medicines was flawed and typically results in patients waiting longer for, and having access to, fewer new cancer drugs when compared with other countries using alternative approaches.
The reports also reveal that over the past decade NICE has been more likely to reject new treatments for cancer than for any other condition – with just 58% of cancer medicines approved compared with 85% for non-cancer treatments during this time.
The healthcare think tank the King’s Fund has now been asked by Janssen to conduct an independent enquiry that will bring together academics, health economists, patient interest groups and others and report to the government on ways it can improve access to all new medicines, not just oncology treatments.
Paul Burstow MP, the former health minister and now chair of the Liberal Democrat health committee, tells PME exclusively that it is time for market access in England to change.
Burstow will not be involved in the King’s Fund report, but has taken a personal interest in the questions being asked around market access. He said: “One of the things that the Abacus and IMS reports have looked at is just what the QALY points to. They found that there are some question marks on the over-reliance on QALY – and health economics in general – as the sole arbiter of whether a drug does, or does not, gain access to the NHS and to patients.
“And what they found was that in reality, different countries around the world using QALY can end up making differing decisions about whether a drug is, or is not, be able to gain entry to patients in the country.
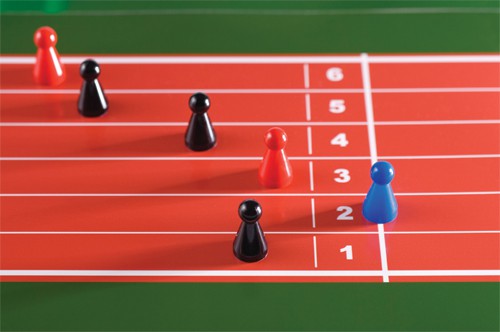
“This is because when using QALYs, just slight tweaks to one area or another can be made, the data sets that are used can materially affect whether something crosses the finishing line in that area, or not.”
Listening to patients
QALY has long been a bugbear for pharma in the UK, which has complained of its ‘coldness’ when it comes to assessing medicines, and a rigidity from NICE that will not see it deviate from its remit on drugs pharma knows to be efficacious but which are just outside the QALY range.
One way to remove this coldness, Burstow says, is to have NICE listen to patients more – something that he feels is currently a perfunctory function of the Institute, rather than being an integral part of its decision-making process.
He explains: “I think there is a case for saying we need to build the perspective of patients more firmly into the way decisions are made. It’s quite striking that in NICE’s own surveys, the patients who sit on health technology appraisal committees say that they don’t always fully understand what their role is to be on those committees, and don’t always feel able to speak up and represent their concerns, and their viewpoint as patients in the process.
“So, there’s definitely something about supporting patients better, about being more supportive in these processes – and this is of course also really important when it comes to rare diseases.”
There is a case for saying we need to build the perspective of patients more firmly into NICE’s decisions
The ABPI, which represents the majority of the major R&D-led pharma firms in the UK, has for a number of years been asking for a top-down reorganisation of NICE that could see some of these changes enacted within its processes.
In fact, NICE had an internal review last year that was designed to add new ‘value-based assessment’ (VBA) policies into the QALY, but the Institute said it was “too complex” to wed these two together, leaving the future of VBA uncertain.
Burstow did not say that the weighting from this policy – such as whether a drug can help get people back to work more quickly, or help reduce costs in social care by keeping patients out of hospital – would still be added to NICE’s remit.
But he did not rule out a political reform from the government on NICE, and market access in England more generally, should the King’s Fund report suggest that this needed to be done.
Pricing
What was not mentioned in the IMS and Abacus reports was whether the prices of new medicines are growing at an unsustainable rate for the government to pay for.
Pricing has in the past year become a bigger issue for payers and the public, and was brought dramatically into the public domain when NICE rejected Roche’s new breast cancer drug Kadcyla last year, saying its £90,000 price tag was nearly twice as expensive as the body would be willing to pay for it.
When asked about pricing, Burstow would not say that drug costs were too high, but suggested new ways of working with pharma to make sure that everyone involved gets the best deal.
He says: “Certainly the reimbursement process does need to reflect those costs of innovation and development that pharma must invest, but I think there is a part here about the role that patient access schemes can play that is more important that just saying ‘prices are too high’.
“Currently, there’s a fairly conservative approach in the UK to the development of patient access schemes, and as a result of that, probably fewer drugs come to market here in a timely fashion than they do in a number of other places, where they are more innovative about the way in which PAS are developed.
“Our PAS system simply seems to be about price cuts whereas others may well look to support infrastructure and other elements; so there are other ways to do this, which could make these deals more attractive.
“Of course the argument against doing this is the more patient access schemes you have, the more complex it becomes for the NHS to manage, and I think that’s one of the things that King’s Fund review will need to consider.”
Commercial in confidence
Almost all of the patient access schemes agreed since 2005, when the ability to negotiate these types of deals first came into place, have been deemed ‘commercial in confidence’, so any price cuts have not been shared with the public.
This is because the UK is a reference country for around 25 other major markets in the world, and discounts made here would be expected to be made elsewhere. But the secrecy around these deals irks health economists and doctor groups, as without knowing how much has been knocked off the price that no one outside NICE, the DH and pharma know if the British taxpayer is getting the best deal.
When asked if these deals should be made public, Burstow said: “In an ideal world, if we could operate an ‘open-book’ approach globally so that every health system was open to every other and we could all see what everyone else is paying, then I would be saying yes, let’s be transparent.
“But we’re not in that place – so for one health economy to be having an open-book approach is very likely to put that country in a disadvantage in terms of gaining early access to new drugs, investment from pharma, and so on.
“I do, however, think there are issues about these commercially confidential agreements that are negotiated between the DH and the pharma industry that do need to be addressed, and that again goes back to having a more innovative approach to them, ie, not just cutting a percentage off the price.
“If we do that, and start asking for pharma to help with infrastructure costs across the board for instance, instead of just cutting price, then organically quite a lot of detail about those things would have to be in the open anyway, because they would be about funding infrastructure that could not go on in secret.”
Burstow also said that he did not think that NICE should ever be the body to discuss PAS with pharma, and that it should remain with staff at the Department of Health, to ensure a democratic and political body is the one negotiating price deals.
The King’s Fund review will likely take place during the summer. PME will be running a special market access and drug pricing supplement in June, after the UK’s General Election, to see what changes pharma should expect from NICE, QALY and market access during the next five-year Parliament.





